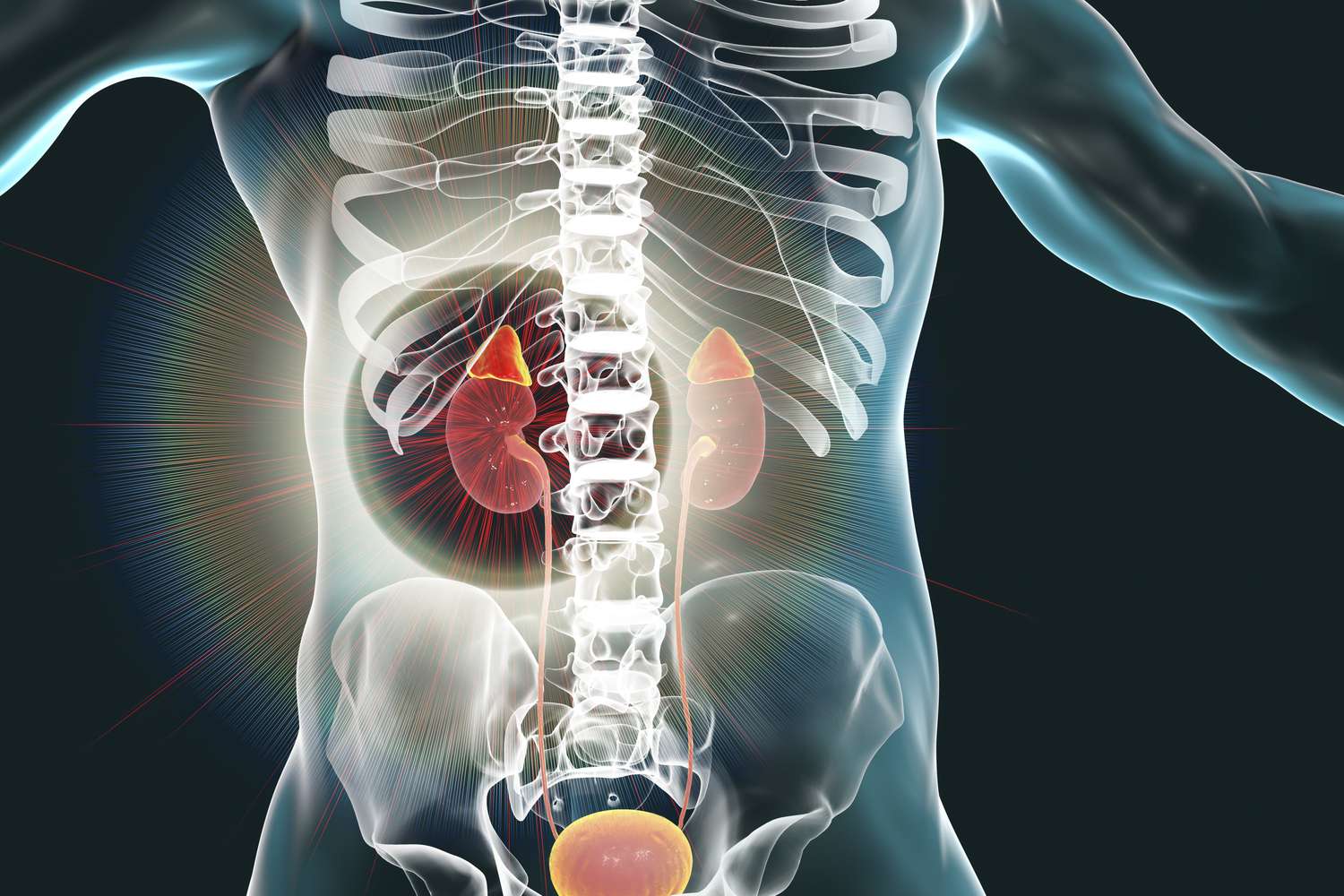
The kidneys are routinely viewed through the narrow, yet critical, lens of filtration and waste excretion. While their function as the body’s sophisticated waste management system—balancing fluid, electrolytes, and acid-base status—is fundamental to survival, this mechanical perspective significantly undervalues their profound and indispensable role as endocrine organs. These bean-shaped structures do far more than simply clean the blood; they are highly active, essential components of several critical hormonal feedback loops, influencing processes that reach far beyond the urinary system. The kidneys are directly responsible for the synthesis of vital hormones, the activation of circulating hormone precursors, and the degradation of hormones, ensuring their appropriate clearance from the bloodstream. This dual function—as both a filter and a gland—makes the kidney central to the stability of blood pressure, the formation of red blood cells, and the structural integrity of the skeletal system. Compromise in renal function, therefore, cascades into systemic hormonal imbalances that affect virtually every major system in the human body.
Essential Components of Several Critical Hormonal Feedback Loops
They are highly active, essential components of several critical hormonal feedback loops, influencing processes that reach far beyond the urinary system.
The kidneys operate as sophisticated endocrine regulators through complex feedback mechanisms involving the brain, adrenal glands, and bone marrow. Their hormonal activity is precisely calibrated to maintain homeostasis under constantly changing physiological conditions. For instance, a drop in systemic blood pressure or blood volume immediately triggers the renal release of renin, a key enzyme that initiates the Renin-Angiotensin-Aldosterone System (RAAS)—a potent hormonal cascade that mandates vascular constriction and fluid retention to restore pressure. Conversely, a prolonged drop in oxygen availability (hypoxia) stimulates the renal synthesis of erythropoietin (EPO), a hormone dedicated entirely to signaling the bone marrow to accelerate the production of new red blood cells. The ability of the kidney to both synthesize and regulate these disparate systems underscores its unparalleled importance as an endocrine hub, constantly adjusting circulating hormone levels to ensure systemic stability.
Blood Pressure Regulation: The Renin-Angiotensin-Aldosterone System (RAAS)
The kidneys are directly responsible for the synthesis of vital hormones, the activation of circulating hormone precursors, and the degradation of hormones.
The most immediate and life-sustaining hormonal role of the kidney is its central function in governing arterial blood pressure through the RAAS. Within the kidney’s juxtaglomerular apparatus, specialized cells sense reductions in afferent arteriole pressure or reduced sodium chloride concentration. In response, these cells secrete the enzyme renin into the circulation. Renin then acts upon angiotensinogen (produced by the liver) to convert it to angiotensin I. This is then rapidly converted to the potent vasoconstrictor, angiotensin II, by the Angiotensin-Converting Enzyme (ACE) primarily found in the lungs. Angiotensin II constricts blood vessels, leading to an immediate rise in blood pressure, and also stimulates the adrenal cortex to release aldosterone. Aldosterone, in turn, acts on the renal tubules to promote the retention of sodium and water, further augmenting blood volume and pressure. The RAAS is, therefore, a textbook example of a multi-organ endocrine axis where the kidney acts as the indispensable initiator and also the final mediator of the entire feedback loop.
Erythropoietin: The Red Blood Cell Commander
A prolonged drop in oxygen availability (hypoxia) stimulates the renal synthesis of erythropoietin (EPO), a hormone dedicated entirely to signaling the bone marrow to accelerate the production of new red blood cells.
The kidney is also the primary site of production for erythropoietin (EPO), a glycoprotein hormone that serves as the crucial stimulus for red blood cell production, or erythropoiesis. The sensing cells within the renal cortex monitor the oxygen levels delivered to the kidney. When oxygen tension drops significantly (as in cases of anemia, high altitude, or chronic lung disease), the renal cells respond by sharply increasing the synthesis and secretion of EPO. Circulating EPO then travels to the bone marrow, binding to receptors on progenitor cells and forcing their differentiation and maturation into functional red blood cells. The failure of this endocrine function—a hallmark of Chronic Kidney Disease (CKD)—is the leading cause of renal anemia, a condition characterized by debilitating fatigue that cannot be corrected by iron supplements alone, but requires therapeutic EPO administration.
Calcitriol: The Active Form of Vitamin D
The kidneys activate circulating hormone precursors, ensuring their appropriate clearance from the bloodstream.
A less appreciated, yet equally vital, endocrine function is the kidney’s role in the metabolism of Vitamin D. The inactive, circulating form of Vitamin D (calcifediol, or 25(OH)D) is produced in the liver. However, it is the kidneys that contain the essential enzyme, 1−α-hydroxylase, which performs the final, activating step to convert calcifediol into the potent, biologically active hormone, calcitriol (or 1,25(OH)2D). Calcitriol is critical for calcium and phosphate homeostasis; it promotes calcium absorption from the gut and regulates its movement in the bone. When renal function declines, the production of calcitriol falls sharply, leading to a condition known as renal osteodystrophy (or Chronic Kidney Disease-Mineral and Bone Disorder), which is characterized by weak bones, fractures, and vascular calcification, demonstrating the profound link between renal hormonal activity and skeletal health.
Interplay with the Parathyroid Hormone (PTH)
The inability to produce adequate calcitriol leads to secondary hyperparathyroidism, a significant complication of advanced renal disease.
The kidney’s role in calcitriol production places it in a tight regulatory loop with the Parathyroid Hormone (PTH), produced by the parathyroid glands. When calcitriol levels fall due to impaired kidney function, intestinal calcium absorption drops, leading to hypocalcemia (low blood calcium). The body attempts to compensate by increasing the secretion of PTH, which is meant to draw calcium from the bones and increase its reabsorption in the tubules. However, the diseased kidney remains unresponsive, unable to produce more calcitriol to suppress this action. This cycle results in secondary hyperparathyroidism, a significant complication of advanced renal disease, where persistently high PTH levels excessively demineralize the skeleton, further contributing to bone disease and chronic systemic inflammation—an intricate endocrine domino effect initiated by renal failure.
Degradation and Clearance of Circulating Hormones
This dual function—as both a filter and a gland—makes the kidney central to the stability of blood pressure, the formation of red blood cells, and the structural integrity of the skeletal system.
Beyond synthesizing hormones, the kidney acts as a crucial site for the degradation and clearance of a vast array of circulating hormones and peptides. Hormones such as insulin, growth hormone, prolactin, and glucagon must be continuously removed from the bloodstream once their biological action is complete to prevent their over-accumulation. The renal tubules are responsible for breaking down and reabsorbing these peptide hormones. In the context of CKD, the kidney’s ability to perform this clearance function is severely compromised. For instance, the reduced clearance of insulin can lead to confusing hypoglycemia in diabetic patients, and the decreased clearance of prolactin can lead to hyperprolactinemia, illustrating how renal failure disrupts not only its own endocrine functions but also the regulatory cycles of multiple other glands across the body.
The Adrenal Cortex and Aldosterone
Aldosterone, in turn, acts on the renal tubules to promote the retention of sodium and water, further augmenting blood volume and pressure.
A specialized element of the RAAS hormonal axis involves the relationship between angiotensin II and the adrenal cortex. When angiotensin II levels are high, it specifically targets the zona glomerulosa of the adrenal cortex, stimulating the synthesis and release of the mineralocorticoid hormone, aldosterone. Aldosterone then circulates back to the renal collecting ducts and distal tubules, where its job is to increase the reabsorption of sodium (Na+) and the excretion of potassium (K+). Since water follows sodium, this action effectively increases total body fluid volume, thus reinforcing the blood pressure increase initiated by the renin release. This intricate, closed-loop system is essential, but it is precisely this mechanism that is targeted by common blood pressure medications like ACE inhibitors, demonstrating the kidney’s role as the pivot point in systemic hypertension.
Renal Prostaglandins and Local Vascular Control
This endocrine hub, constantly adjusting circulating hormone levels to ensure systemic stability.
In addition to systemic hormones, the kidneys produce powerful local hormones known as prostaglandins. These are lipid compounds that act primarily as local mediators, particularly influencing intra-renal blood flow. Prostaglandins, like prostaglandin E2 and prostacyclin, are vasodilators, meaning they cause the blood vessels within the kidney to relax and widen. This local action is critical, especially when systemic blood pressure drops, as the prostaglandins ensure that blood flow to the renal glomeruli is maintained, protecting the crucial filtration rate. The therapeutic consequence of this is seen when patients take non-steroidal anti-inflammatory drugs (NSAIDs); these drugs inhibit prostaglandin synthesis, which can dangerously constrict renal blood vessels and lead to acute kidney injury, showcasing the sensitivity of this local hormonal system.
The Future of Renal Endocrinology and Therapy
Compromise in renal function, therefore, cascades into systemic hormonal imbalances that affect virtually every major system in the human body.
The growing understanding of the kidney as a central endocrine organ is revolutionizing the management of chronic renal failure. The focus is shifting beyond simple dialysis to targeted hormonal replacement and modulation. This includes the routine use of recombinant EPO therapy to manage anemia and the therapeutic administration of calcitriol analogs to control secondary hyperparathyroidism and bone disease. Future therapeutic strategies are exploring ways to modulate hepcidin and other renal peptides to more precisely control systemic iron levels and inflammation. This expanding field of renal endocrinology promises more integrated, systemic treatments that specifically address the cascading hormonal failures that define advanced kidney disease, offering a more holistic approach to patient care that recognizes the kidney’s true multifunctional complexity.