Have you ever wondered why some people suddenly develop kidney problems even when they appear otherwise healthy? Many individuals feel fine for years before quiet inflammation begins affecting how the kidneys filter waste. According to our editor’s research, autoimmune conditions often trigger slow and subtle damage before noticeable symptoms appear. These early changes may alter filtration rates, fluid balance and electrolyte levels. People sometimes overlook mild signs because they feel temporary or unrelated. Understanding how autoimmune activity influences the kidneys can help you stay one step ahead and notice patterns before they gain momentum.
What makes kidneys vulnerable to autoimmune activity?
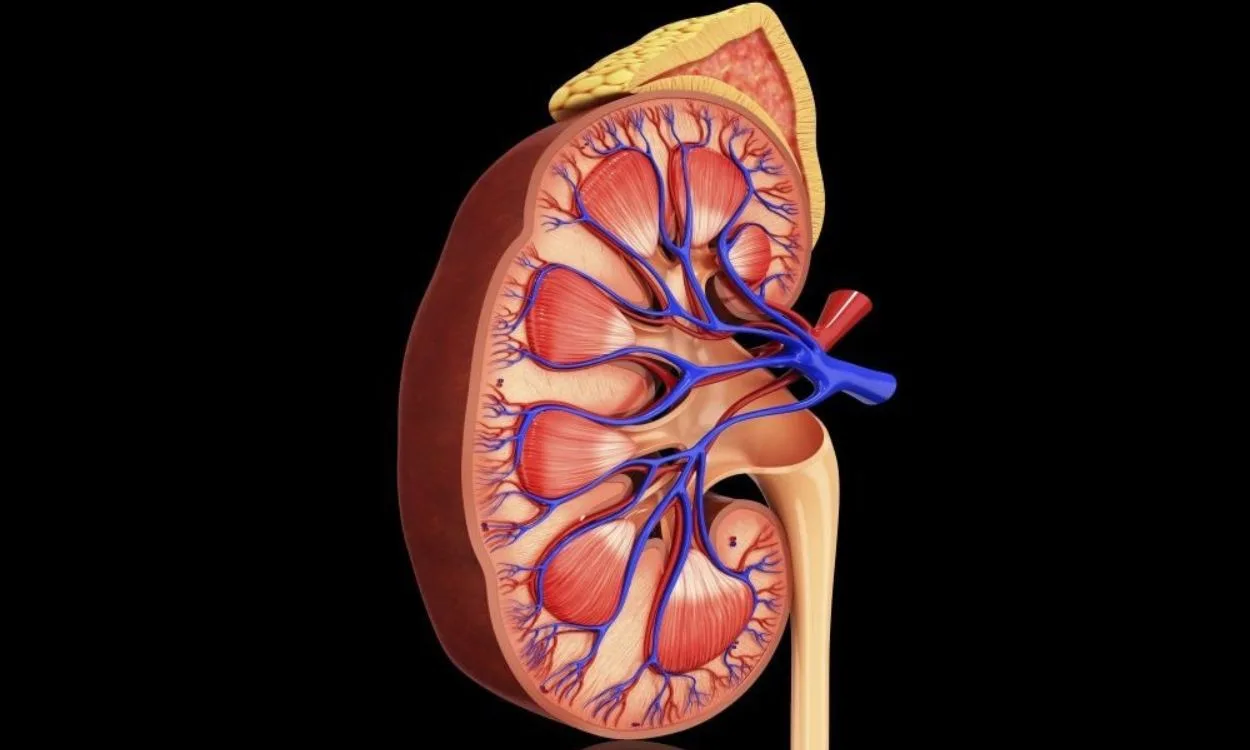
The kidneys contain delicate filtration units. These units respond quickly to inflammation. Autoimmune diseases often target tissues with rich blood flow. As a result of our editor’s reviews, the kidneys become common sites of immune disruption. Antibodies may mistakenly attack kidney structures. This reaction triggers swelling and cellular stress. The filtration barrier becomes less stable. Waste removal slows over time. Fluid and minerals shift unexpectedly. These small changes accumulate quietly. Understanding kidney vulnerability helps you recognize early warning signs.
How do autoimmune diseases trigger kidney inflammation?
Autoimmune diseases confuse the immune system. The body identifies its own proteins as threats. This response creates inflammatory chemicals. These chemicals enter the bloodstream quickly. According to our editor’s research, the kidneys receive large volumes of blood each minute. This exposes them to circulating inflammatory markers. The immune system may then target kidney tissue directly. Inflammation thickens the filtration membrane. This reduces flow and increases pressure. Damaged areas allow protein leakage. These reactions develop gradually. Understanding inflammation patterns helps reveal early kidney involvement.
Why is lupus closely linked to kidney damage?
Lupus frequently affects the kidneys. Doctors call this lupus nephritis. According to our editor’s research, nearly half of lupus patients develop kidney involvement. Lupus creates widespread antibody activity. These antibodies form circulating complexes. The kidneys trap these complexes during filtration. This triggers high levels of inflammation. Lupus nephritis appears in several forms. Some forms cause rapid changes. Others move slowly over years. Symptoms may appear mild at first. Swelling in the legs may be the first sign. Understanding lupus patterns supports earlier medical decisions.
What happens when rheumatoid arthritis impacts the kidneys?
Rheumatoid arthritis primarily affects joints. However autoimmune chemicals move through the bloodstream. As a result of our editor’s reviews, long lasting inflammation can influence kidney function. Certain medications used for arthritis may also stress the kidneys. Some patients develop amyloidosis. This condition causes abnormal proteins to collect in organs. The kidneys filter these proteins poorly. This leads to swelling and high protein urine. Patients may feel more tired. Some notice appetite changes. Understanding arthritis complications encourages careful monitoring.
How does vasculitis harm kidney tissue?
Vasculitis inflames blood vessels. The kidneys depend on healthy vessels for filtration. According to our editor’s research, inflamed vessels reduce oxygen and nutrient flow. This starves kidney tissue slowly. Damaged vessels may leak. Fluid escapes into surrounding tissue. This increases swelling and pressure. Some forms of vasculitis progress rapidly. Doctors monitor kidney function closely. Early treatment helps limit damage. Managing vessel inflammation protects long term filtration health. Understanding vasculitis effects highlights the need for quick evaluation.
Why is protein in urine a common warning sign?
Protein should remain in the bloodstream. Healthy kidneys prevent protein leakage. Autoimmune inflammation weakens this barrier. As a result of our editor’s reviews, protein in urine becomes a frequent early clue. Patients may not notice visible changes. Doctors detect protein through simple tests. High levels indicate structural stress. Persistent leakage reflects ongoing inflammation. Protein loss can cause swelling. Low blood protein affects energy levels. Identifying this sign early improves treatment planning. Understanding urine signals supports early detection.
How do autoimmune diseases change filtration speed?
Filtration speed reflects kidney performance. Autoimmune inflammation slows efficiency. According to our editor’s research, inflammatory swelling narrows filtration pathways. This reduces flow and increases pressure. Doctors measure filtration through estimated rates. Declining rates reveal stress. Some patients develop rapid drops. Others show slow declines. Tracking changes over time helps identify autoimmune influence. Early detection improves long term outcomes. Understanding filtration speed encourages routine testing.
Why do some patients experience high blood pressure?
Kidneys regulate blood pressure. Damaged kidneys struggle with this role. As a result of our editor’s reviews, autoimmune inflammation often raises blood pressure. Swollen tissue disrupts fluid balance. Hormone levels shift unpredictably. Narrowed vessels increase resistance. High pressure damages filtration units further. This creates a cycle of strain. Patients may not notice early pressure changes. Regular monitoring becomes essential. Understanding blood pressure patterns supports timely intervention.
How do symptoms differ among autoimmune diseases?
Each autoimmune disease affects the kidneys uniquely. Lupus may cause swelling and foamy urine. Vasculitis may cause fever and rapid decline. According to our editor’s research, some conditions remain silent for long periods. Patients may only feel mild fatigue. Appetite loss may appear late. Joint pain or skin changes may accompany kidney stress. Overlapping symptoms create confusion. Doctors use testing to clarify patterns. Understanding symptom diversity encourages careful observation.
Why do doctors rely heavily on blood and urine tests?
Testing reveals silent inflammation. Kidney changes appear quickly in lab values. As a result of our editor’s reviews, doctors track multiple markers. Creatinine reflects filtration strength. Protein indicates structural damage. Blood cell levels show inflammation. Testing over time reveals trends. Trends guide therapy decisions. Early changes may respond well to treatment. Testing supports precision and safety. Understanding test importance motivates regular follow ups.
How does imaging support autoimmune kidney assessment?
Imaging reveals structural changes. Ultrasound provides details about kidney size. According to our editor’s research, inflammation may cause swelling. Some conditions shrink kidney tissue slowly. Imaging highlights blood flow patterns. Blood flow reveals vessel inflammation. Scarring appears in later stages. Imaging supports diagnosis when symptoms remain unclear. Combined with lab results, imaging provides a complete picture. Understanding imaging value strengthens early assessment.
What treatment options reduce autoimmune kidney damage?
Treatment depends on the autoimmune condition. Doctors aim to calm immune activity. As a result of our editor’s reviews, medications reduce inflammation. Some drugs protect kidney structures. Blood pressure control reduces strain. Diet plays a small supportive role. Low sodium intake helps fluid balance. Adequate hydration supports filtration. Regular monitoring improves safety. Early therapy prevents irreversible changes. Understanding treatment goals encourages adherence.
Why does early diagnosis improve long term outcomes?
Autoimmune kidney issues develop quietly. Early diagnosis stops progression. According to our editor’s research, untreated inflammation accelerates decline. Small injuries accumulate. These injuries reduce filtration reserve. Once lost, reserve does not return. Early intervention preserves remaining function. Doctors adjust treatment during flare cycles. Early care stabilizes long term health. Understanding timing reinforces proactive decisions.
How can patients protect kidney health during flares?
Flares increase inflammation levels. Smart habits protect kidney tissue. As a result of our editor’s reviews, hydration becomes essential. Patients should monitor blood pressure regularly. Avoiding unnecessary medication strain helps. Rest supports recovery. Stress management lowers immune activation. Doctors may advise slower physical activity. Monitoring symptoms during flares prevents surprise changes. Understanding flare behavior promotes stability.
Why do some autoimmune conditions require long term kidney monitoring?
Autoimmune diseases fluctuate. Kidney involvement may return unexpectedly. According to our editor’s research, long term monitoring detects recurrence. Testing becomes part of routine health care. Monitoring includes checking urine, blood and pressure. Imaging may appear occasionally. Doctors adjust treatment based on results. Long term stability depends on consistent follow up. Understanding monitoring needs supports lifelong awareness.
How do lifestyle choices influence autoimmune kidney outcomes?
Lifestyle impacts inflammation. Nutrition influences immune activity. As a result of our editor’s reviews, balanced diets reduce stress. Exercise supports circulation. Adequate sleep improves immune regulation. Avoiding smoking protects vessels. Limiting alcohol supports filtration. Stress management reduces flare risk. Healthy routines complement medical care. Understanding lifestyle influence encourages better habits.
What questions should patients ask their doctors?
Clear communication improves outcomes. Patients should ask about inflammation markers. According to our editor’s research, understanding lab results reduces anxiety. Asking about flare signs helps with early detection. Patients may ask how medications protect kidneys. Clarifying long term expectations builds confidence. Understanding these questions empowers proactive decisions.