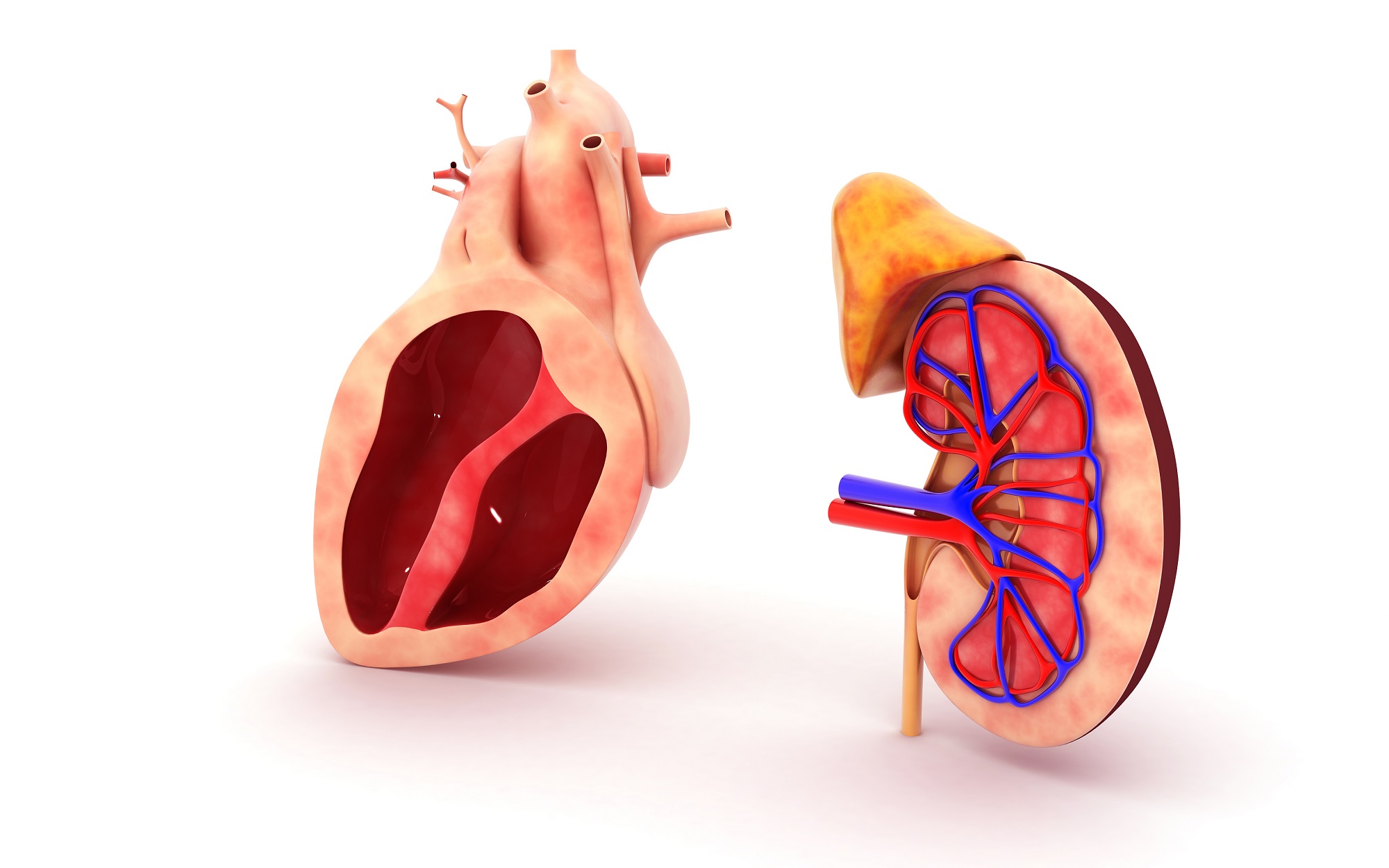
The heart and kidneys work as a connected system. One affects the other continuously. When the heart weakens, kidneys receive less blood. When kidneys decline, toxins build up and strain the heart. It’s a cycle. You may notice fatigue, swelling, or blood pressure issues. But the root cause often involves both organs. One condition may come first. The second often follows soon after.
High blood pressure is a major shared risk factor for both heart and kidney problems
Hypertension damages blood vessels. In the heart, this increases workload. In the kidneys, it affects filtration. Over years, this leads to heart failure or chronic kidney disease. It may begin silently. Many people don’t feel symptoms. But damage continues beneath the surface. Treating blood pressure early helps protect both organs. Medication, diet, and exercise play major roles.
When kidney function drops, excess fluid and waste increase the burden on the heart
Healthy kidneys filter out sodium, water, and toxins. As function drops, these remain in circulation. The heart must pump harder to move this heavier blood. Fluid builds in the lungs and legs. Blood pressure rises. Heart strain increases. This leads to shortness of breath and swelling. Many patients assume it’s a heart issue. But the kidneys are often involved too.
Heart failure reduces kidney perfusion, which worsens filtration and leads to further fluid retention
The kidneys rely on steady blood flow to function. In heart failure, blood output drops. Kidneys detect low pressure and hold onto salt and water. It’s a protective mechanism—but it backfires. More fluid enters the bloodstream. The heart strains further. Filtration declines. Creatinine rises. This creates a feedback loop. Heart and kidney damage accelerate together.
Diabetes often accelerates damage to both the cardiovascular and renal systems simultaneously
Uncontrolled blood sugar harms arteries. It narrows vessels in the heart and the kidneys. Over time, protein leaks into urine. Kidney filtration declines. Meanwhile, fatty buildup increases heart risk. Many diabetic patients develop both kidney disease and heart problems. The combination is dangerous. Tight glucose control slows progression. Early screening is essential.
Chronic inflammation and oxidative stress damage tissues in both the heart and the kidneys
Inflammation isn’t visible—but it’s destructive. It stiffens arteries and scars kidney tissue. Oxidative stress worsens this damage. It alters cell function and structure. These forces act slowly. Years pass before symptoms appear. But the underlying damage is deep. Lifestyle changes reduce inflammation. Antioxidants, exercise, and sleep help support recovery. Medications may also help reduce long-term harm.
Fluid overload and electrolyte imbalances from kidney disease can trigger arrhythmias and heart stress
Kidneys regulate potassium, calcium, and fluid balance. When they fail, these levels change unpredictably. High potassium triggers arrhythmias. Sodium shifts cause swelling and confusion. These chemical imbalances impact heart rhythm directly. The result may be palpitations, fainting, or even cardiac arrest. Managing electrolytes becomes critical in late-stage kidney disease. Dialysis may be needed.
Many medications used to treat one condition must be adjusted to protect the other
Some heart drugs affect kidney filtration. Some kidney medications change blood pressure. The overlap is delicate. Diuretics help heart failure but can dry kidneys. ACE inhibitors help kidneys but lower pressure. Each adjustment has consequences. That’s why specialists often coordinate care. Cardiologists and nephrologists work together. The balance isn’t fixed—it evolves with the patient’s condition.
Lifestyle changes that protect the heart usually benefit the kidneys as well
Diet affects both organs. Less salt reduces blood pressure and fluid retention. Regular exercise improves circulation and metabolism. Smoking cessation helps arteries and kidney tissues. Weight loss improves control of diabetes and hypertension. These changes don’t reverse disease—but they slow its progress. Small actions build over time. Both systems respond better when the whole body is cared for.
Monitoring both cardiac and renal function helps detect silent decline before symptoms appear
Damage often begins quietly. Regular checkups are critical. Blood tests show kidney filtration. Urine tests detect protein leaks. Echocardiograms assess heart strength. Blood pressure reveals vascular stress. These data points work together. Alone, they’re limited. Together, they show trends. Early detection leads to better outcomes. Preventive care often begins before you feel sick.